uMETHOD’s AI software helps doctors assess and reduce risk of falls among patients with cognitive decline
By John Q. Walker, Ph.D
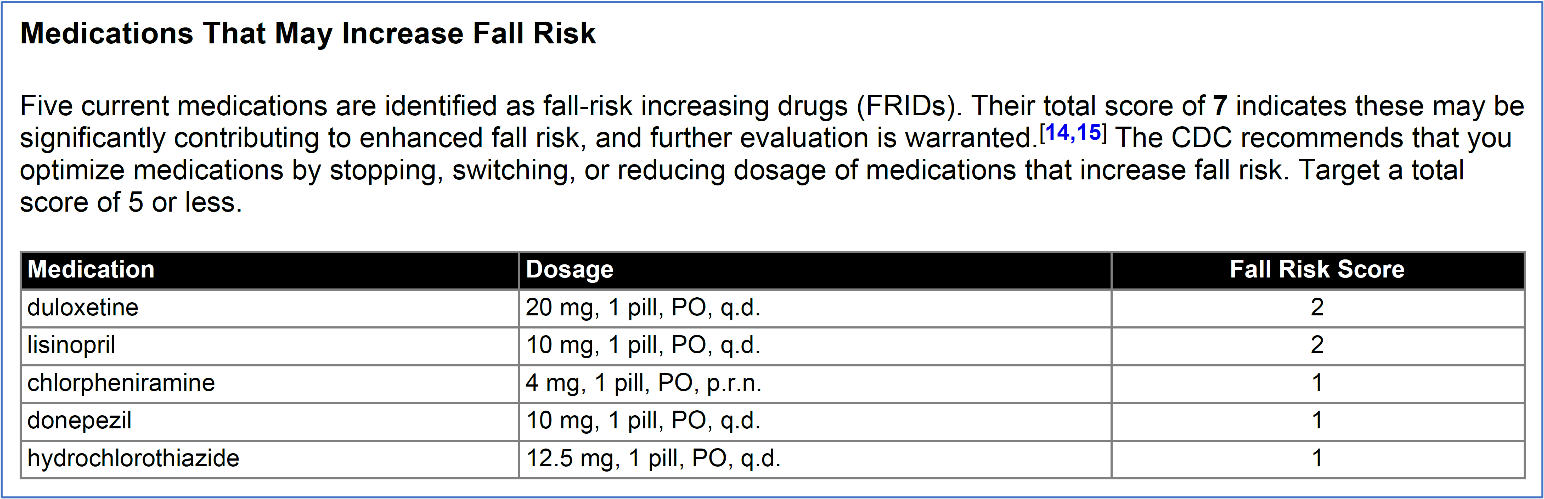
uMETHOD Health is a technology company in Research Triangle Park, North Carolina, focused on treating the causes of complex diseases. Its RestoreU METHOD uses patented artificial-intelligence (AI) software to identify the underlying factors that drive someone’s cognitive decline. This software generates personalized care plans on how to prevent, slow, or even roll-back the progression of cognitive decline. The software now identifies all the drugs someone may be taking that increase their likelihood of falling, showing the “fall risk score” for each medication, as well as their total score.
Falls are the leading cause of injury among those over 65 years old, and consequently result in high healthcare demand. This includes direct medical treatment, long-term rehabilitation and pain management, and social consequences. More than a third of older adults fall each year, with half of those falling two or more times per year. Fall accidents are even more common in older people residing in nursing homes, with an incidence rate approaching 50%.
Injuries occur in about 10% of falls. Over 3 million people are treated in US emergency departments annually for these fall injuries. Total healthcare costs are high, due to the high incidence of falls and the high costs per incident. For example, the direct healthcare costs per patient with a hip fracture can exceed $20,000. In 2018, for non-fatal falls, Medicare paid approximately $28.9 billion, Medicaid $8.7 billion, and private and other payers $12.0 billion. Overall medical spending for fatal falls was estimated to be $754 million.
Older women are disproportionately affected. Rates for injury diagnoses were generally higher among women, most notably for fracture, which was 2.2 times higher than the rate among men. The hospitalization rate for women was 1.8 times that for men.
Fall-risk increasing drugs (FRIDs) have been described in research that spans the past decade-and-a-half. This includes the classic book by Janice Morse and the work documented by Beasley et al. in 2009, showing how the risk for falls would be scored for each medication. The risk from medications was suggested in the Beers Criteria in 2012 and 2019 (which is cited by the CDC), as well as in recent research. uMETHOD’s work supersedes these, translating this body of medical research into software that comprehensively automates the analysis for each patient. For each care plan, a table of 825 FRIDs are assessed, spanning 105 pharmacologic classes – across generics, brands, and combination formulations.
It isn’t falls themselves that accelerate cognitive decline, but the outcomes of falls can.
- Falls are often the reason that someone progresses from an active lifestyle to constrained mobility – which, in turn, leads to far less activity and exercise. Nothing rebuilds brain cells like exercise, and lack of exercise and general physical activity is a factor accelerating the progression to Alzheimer’s disease – a factor that’s hard to turn back.
- People with injuries due to falls are likely to be in pain, and are far more likely to be taking additional medications, like opioids, to relieve the pain. All opioids both increase anticholinergic cognitive burden (ACB, known as “brain fog”) and fall risk – accelerating a vicious cycle.
- Falls can lead to broken bones or other internal injuries, sometimes requiring surgery. Certain types of anesthesia used during surgery are known to cause irreversible cognitive decline.
- Many falls result in traumatic brain injury (TBI). Brain trauma is another of the dozens of factors that accelerate the progression of Alzheimer’s disease. Some falls among the elderly are severe enough to lead directly to death; falls are one of the primary reasons someone dies *with* Alzheimer’s disease.
- The genetics of ApoE4 accelerate one’s progression to Alzheimer’s disease. Those with ApoE4 have heightened susceptibility to head traumas and chronic traumatic encephalopathy (CTE) (that is, these traumas increase the rate of Alzheimer’s progression).
- A fall can be the trigger for the move from independent living in one’s home to assisted living – a horrible and costly step for the person themselves, as well as their family and loved ones.
The fall risk for every known prescription and over-the-counter drug can be scored on a scale of 0 to 3, where 0 means no enhanced risk and 3 means the drug induces the highest possible risk. Cumulative scores higher than 5, across all of someone’s current medications, should be avoided if possible, and should be pursued aggressively by their physician.
Here’s an example of what the fall risk assessment might look like, in the front of a RestoreU care plan: